Patients Who Underwent Lung Transplantation at Cedars-Sinai Experienced 1-Year Survival Rates Above National Average
A new report on lung transplantation success rates confirms that Cedars-Sinai patients experienced one-year survival outcomes of 91.49%, an achievement above the national average of 89.46%.
The data—compiled by the Scientific Registry of Transplant Recipients—provides a hopeful prognosis—and options—for patients requiring the complex yet lifesaving surgery.
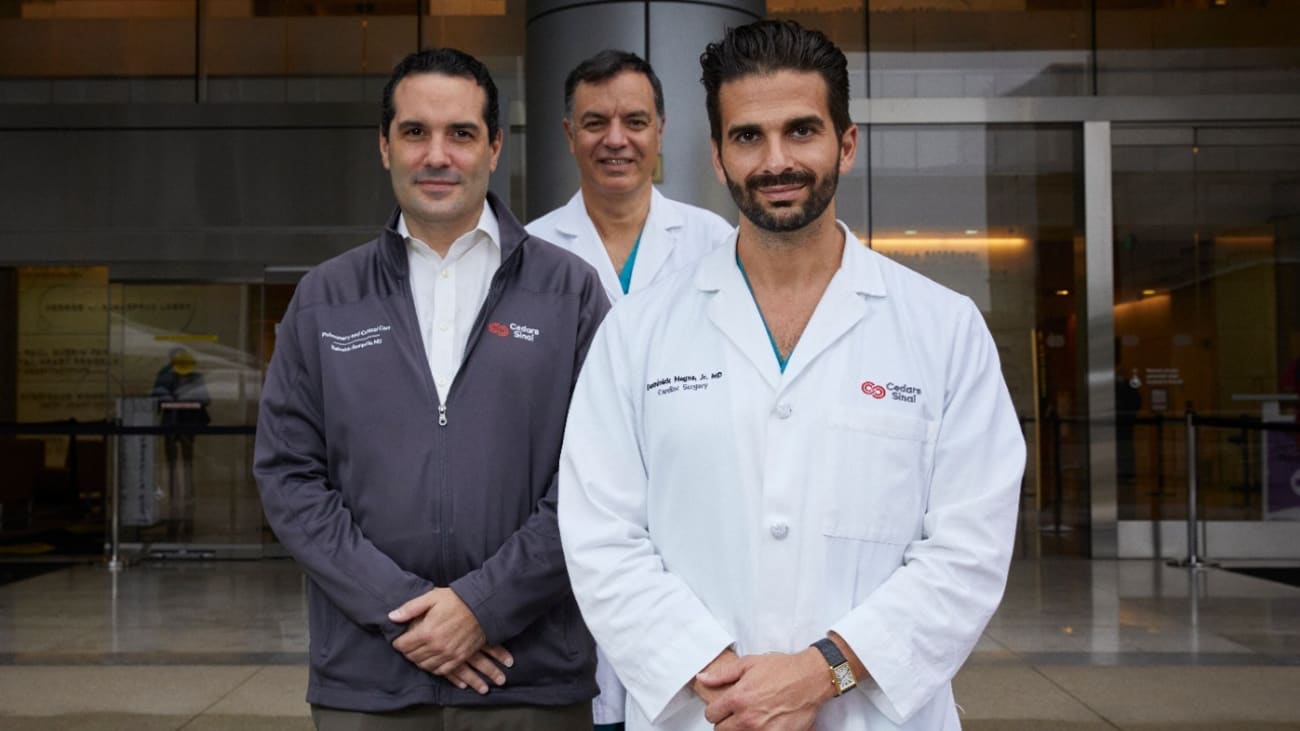
Lung transplantation at Cedars-Sinai—a collaboration between the Smidt Heart Institute and the Comprehensive Transplant Center—is characterized by innovations that are changing the landscape of cardiothoracic surgery and care.

Joanna Chikwe, MD
“Our team is known for pushing the boundaries and successfully treating patients that most other programs aren’t able to help,” said Joanna Chikwe, MD, chair of the Department of Cardiac Surgery in the Smidt Heart Institute at Cedars-Sinai, who oversees lung transplant surgery. “We offer a path forward for patients left with few options, doing so with cutting-edge technologies and surgical techniques and world-class clinical care.”
In 2021, a Cedars-Sinai patient underwent what is considered to be the nation’s first minimally invasive double lung transplant surgery using a novel technique and resulting in an incision no longer than a driver’s license. In addition to faster recovery times, patients undergoing the minimally invasive procedure often experience less pain and shorter hospital stays.
By 2022, Cedars-Sinai surgeons began offering robotic-assisted minimally invasive lung transplantation—an advance that has further accelerated healing while shortening hospital stays.
“Our minimally invasive approaches are unique in the world, and allow us to successfully transplant patients who are often dismissed by other institutions,” said Pedro Catarino, MD, director of Aortic Surgery in the Smidt Heart Institute and the visionary behind these procedures. “We have had great success in patients who are frail and complex, including those who need multi-organ transplants.”
Dominick Megna, MD, surgical director of the Lung Transplant Program, stressed the team’s expertise in also treating patients who are immunologically sensitized, and those who have irreversible lung damage from the virus that causes COVID-19.
“COVID-19 was, in fact, a key factor in how we now approach lung transplantation,” said Megna.
Amy Yamaguchi, a then-34-year-old first-time-expectant mother, was Cedars-Sinai’s first COVID-19 lung transplant recipient.
Yamaguchi was 36 weeks pregnant when she was diagnosed with COVID-19 and underwent emergency cesarean section. After her daughter’s birth, she was transferred from her local hospital to Cedars-Sinai without ever having held her firstborn child. Yamaguchi was immediately placed on ECMO—a machine that helps pump a patient’s blood through an artificial lung.
“We learned, very quickly, that in carefully selected patients, we could use ECMO as a bridge to lung transplantation,” said Megna. “Since the beginning of the pandemic, we have performed 22 lung transplants for COVID-19 patients, which have contributed to our successful survival outcomes.”
These experiences led the team to perform a seminal analysis, published in The New England Journal of Medicine, suggesting that lung transplantation could help patients with severe, irreversible lung damage from COVID-19.
Pre- and post-surgery, lung transplant patients benefit from a team of medical experts, led by Reinaldo Rampolla, MD, medical director of the Lung Transplant Program. With his expertise in pulmonary diseases and a unique approach to patient care, he ensures that each lung transplant patient is heard, seen and supported.
“Our program is successful, not only because of our technical abilities, but also because of teamwork,” said Rampolla. “There’s camaraderie among the lung transplantation team—and it brings out the best in each of us.”
Chikwe, who has the unique opportunity to oversee lung transplantation at Cedars-Sinai, agrees that this camaraderie drives success.
“We are leveraging one of the greatest teams in cardiothoracic medicine,” said Chikwe, the Irina and George Schaeffer Distinguished Chair in cardiac surgery. “This is where excellence happens every day.”
Read more from the Cedars-Sinai Blog: The New Lung Cancer Landscape
