By Nicole Davis, PhD
Pairing multiple drugs together to synergistically destroy a patient's tumor has become a common approach to cancer treatment. But determining which of the hundreds of available cancer drugs work best together is often a monumental challenge. Sometimes, promising matches can emerge through trial and error, but increasingly, researchers are harnessing a deep scientific understanding of how drugs work to identify powerful combinations.
That science-driven approach has enabled researchers from Dana-Farber's Division of Gynecologic Oncology to identify a potential drug partner for olaparib, which blocks a key protein — called poly (ADP ribose) polymerase, or PARP — and has transformed the treatment of some forms of cancer, especially ovarian cancer. Their decade-long effort has now culminated in an international, multi-site phase 3 clinical trial that is testing the effectiveness of the drug pair (olaparib and a drug called alpelisib) in hundreds of ovarian cancer patients with recurrent platinum resistant cancer, a critical step toward bringing this promising treatment option to the clinic.
Promising Data Shows Potential for PARP and PI3K
The story begins in April 2011, when intriguing data was presented at a meeting of Stand Up To Cancer (SU2C) researchers. This collaborative "Dream Team" was exploring the role of an important protein, known as phosphoinositide 3-kinase or PI3K, in breast and gynecologic cancers using mouse models. Dana-Farber's Ursula Matulonis, MD, was a member of the team, together with other prominent cancer researchers including Lewis Cantley, PhD (then at Cornell University, but now at Dana-Farber as of February 2022), Gerburg Wulf, MD, PhD (of Beth Israel Deaconess Medical Center), and José Baselga, MD, PhD (a breast cancer specialist who passed away in 2021).
"Their data was really impressive," said Dr. Matulonis, who is chief of the Division of Gynecologic Oncology. "The laboratory experiments showed that a drug that blocks PI3K could work synergistically with a PARP inhibitor to kill breast cancer cells — both the cells that carried mutations in the BRCA genes as well as those that did not harbor the BRCA mutation."
At the time, PARP inhibitors were known to work particularly well in BRCA-mutated ovarian cancers, in which PARP inhibitors were first tested. That's because these cells harbor defects in one of several pathways for repairing DNA. PARP inhibitors block a different DNA repair pathway, delivering a fatal blow known in scientific parlance as synthetic lethality.
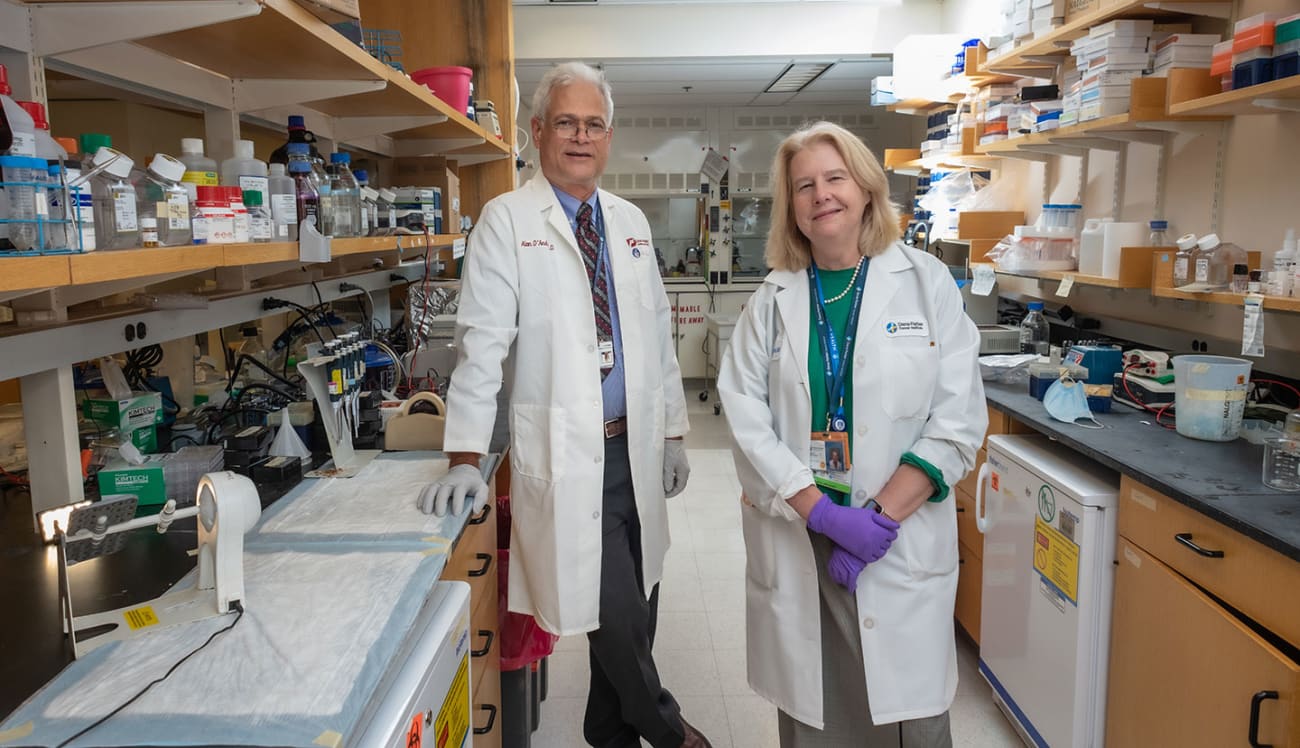
"If a tumor is deficient in one DNA repair pathway, like the BRCA pathway, it is now hyper-dependent on other DNA repair pathways," explained Alan D'Andrea, MD, director of the Susan F. Smith Center for Women's Cancers and the Center for DNA Damage and Repair at Dana-Farber. "If you can inhibit one of those other pathways, you'll kill the cancer. That's the fundamental concept of synthetic lethality."
While this concept provided an explanation for why PARP inhibitors worked so well in BRCA-mutated tumors, it leaves unanswered another big question: How to render other tumors, which do not carry mutations in the BRCA genes, sensitive to this drug combination? It's a particularly pressing question for patients with ovarian cancer, many of whom do not harbor mutations in these genes.
"That was really one of the questions we were trying to figure out; how could we make non-BRCA mutated cancer cells sensitive to PARP inhibitors?" said Dr. Matulonis. "The Dream Team data suggested a way to do that."
A Deeper Exploration
Spurred by this early data, Dr. Matulonis and her colleagues collaborated with Novartis and AstraZeneca to launch a phase 1 clinical trial, which combined a recently developed PI3K inhibitor, called BKM120, with olaparib. The trial included nearly 70 patients, many with ovarian cancer and some with breast cancer, to test the safety and effectiveness of this drug combination.
Although the researchers saw some signs that the combination was effective, they also noticed some significant side effects, particularly in the central nervous system. Because the results were so promising, the team turned to another PI3K inhibitor — called BYL719, or alpelisib — which does not have CNS toxicities.
 Panagiotis Konstantinopoulos, MD, PhD
Panagiotis Konstantinopoulos, MD, PhD
Alpelisib was created by Novartis in an effort to develop PI3K inhibitors that act with greater specificity than BKM120. Unlike its predecessor, alpelisib does not cross the blood-brain barrier, making it less likely to cause central nervous system side effects. Dr. Matulonis and her colleagues, including Panagiotis Konstantinopoulos, MD, PhD, director of translational research in the Division of Gynecologic Oncology and co-director of the The Mellen and Eisenson Family Center for BRCA and Related Genes, thought it might be a better match with olaparib. As a result, the trial was amended.
"I wrote an amendment to the trial, and in 2014, we began testing the combination of alpelisib and olaparib," recalled Dr. Matulonis.
A Second 'Dream Team' Pushes Forward
Meanwhile, as these early clinical trials were unfolding, scientists in the laboratory were digging deeper into the molecular actions of PI3K inhibitors. By understanding how these drugs work in the body, they hoped to learn more about which combinations might be most effective.
"Looking back on the history of alpelisib, it became clear that if you expose a cancer cell to the drug, you'll not only block PI3K, but you'll also interfere with the DNA repair pathway that's controlled by BRCA," said Dr. D'Andrea. In 2015, he was chosen to lead a new SU2C Dream Team, this one focused on the role of DNA repair pathways in ovarian cancer. A major goal of that team was to uncover ways to make PARP inhibitors work in a broader swath of ovarian cancer patients. Matulonis, who was a member of this Dream Team, and her colleagues collaborated to pursue their clinical trial.
As more laboratory data emerged, scientists determined that alpelisib, through its effects on DNA repair, could in fact sensitize cells to PARP inhibitors. "What I love about this story is that there was a real rationale for combining alpelisib with a PARP inhibitor," said Dr. D'Andrea. "You treat with one drug and it makes the cancer more sensitive to the second drug."
Intriguing Evidence of the Therapy's Potential
In late 2016, Dr. Matulonis, Dr. Konstantinopoulos, and colleagues finished enrolling patients with ovarian cancer in the phase 1 trial of alpelisib and olaparib. Although the primary goal of the study was to identify the ideal drug dosages and evaluate safety, the team saw some intriguing evidence of the drug combination's power and anti-cancer responses.
"The study showed very good anti-cancer activity in patients with platinum-resistant ovarian cancer," said Dr. Konstantinopoulos, who was first author of the study, which was published in Lancet Oncology in 2019. "What was also remarkable is that among the patients who responded to the treatment, more than 30% did not carry BRCA mutations."
Based on these findings, Novartis is now sponsoring an international phase 3 clinical trial, known as EPIK-O, to study the effectiveness of olaparib and alpelisib in patients with ovarian cancer. The trial, led by Dr. Konstantinopoulos, began enrolling patients earlier this year. "We hope that over the next few years we'll be able to learn more about the effectiveness of this drug combination in ovarian cancer," he said.
In the meantime, several other potential drug partners for olaparib and other PARP inhibitors are being investigated, too. (See our related article on the next chapter of PARP inhibitors.)
Looking back on the road they've traveled, the Dana-Farber team sees collaboration, catalytic funding, and perseverance as some of the keys to their success.
"It was really Dr. Matulonis' persistence, and also two consecutive Stand Up to Cancer grants, which helped bring this drug combination to fruition," said Dr. D'Andrea.
"This is team science at its best," added Dr. Matulonis. "It's been gratifying to see the science mature and lay the groundwork for a phase 3 study. Of course, more work lies ahead and we're very eager to see where it leads us."